Imagine you’re driving through a bustling city street, and suddenly a smell wafts in through your car window, reminding you of your favourite food. Instantly, you’re transported to memories of enjoying that dish, and soon, you’re craving it. The brain’s chemistry is powerful and capable of creating lasting memories, emotions, and cravings. This is the same mechanism that plays into addiction, where substances alter the brain’s natural chemistry, creating cycles of dependency. In this blog, we’ll explore “The Chemistry of Addiction: How Substances Affect the Brain,” shedding light on how drugs, alcohol, and even certain behaviours can hijack our brain’s reward system.
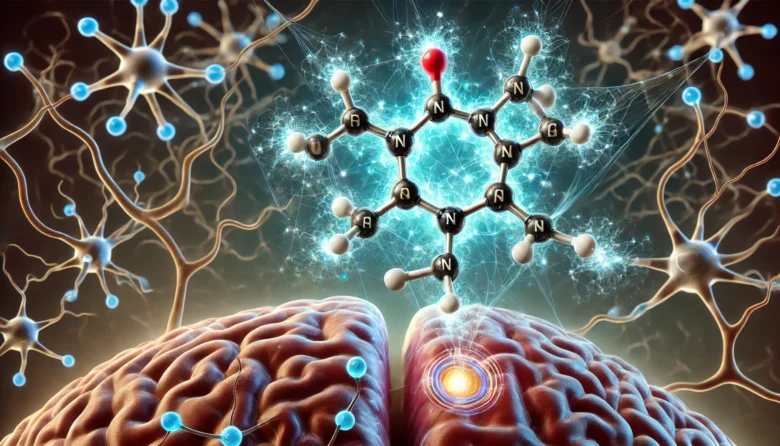
The Brain’s Reward System: Dopamine in Action
At the centre of addiction is a small but powerful neurotransmitter called dopamine. Often referred to as the “feel-good” chemical, dopamine is part of the brain’s reward system, which is designed to reinforce behaviours essential for survival, like eating or socializing. When we experience something pleasurable, our brain releases dopamine, creating feelings of happiness and satisfaction.
But what happens when substances like drugs or alcohol enter the picture? Substances like opioids, nicotine, or alcohol cause an exaggerated release of dopamine, flooding the brain with intense feelings of pleasure or euphoria. This powerful surge of dopamine is far beyond what natural experiences like food or social interactions can produce.
For example, someone using cocaine might feel an intense rush of euphoria due to a massive release of dopamine, which creates a lasting memory in the brain. The brain quickly learns to associate the substance with this feeling of extreme pleasure, making the user want to repeat the experience. This is where addiction begins to take root.

Tolerance and Dependency: The Brain’s Adaptation
As the brain continues to experience these artificial dopamine surges, it starts to adjust. Over time, the brain reduces its natural production of dopamine, and the receptors that respond to dopamine become less sensitive. This is known as tolerance. The person then needs more of the substance to achieve the same pleasurable feeling, leading to increased use.
For example, someone who regularly drinks alcohol might find that the initial few drinks no longer provide the same buzz, leading them to drink more to chase the same effect. This leads to physical dependency, where the brain relies on the substance to maintain normal dopamine levels.
Without the substance, the brain struggles to balance itself, causing withdrawal symptoms—headaches, irritability, nausea, or anxiety. This pushes the individual to use the substance again, not just for pleasure, but to avoid the discomfort of withdrawal.
The Role of Other Neurotransmitters: GABA and Glutamate
While dopamine plays a central role in addiction, it’s not the only neurotransmitter involved. Gamma-aminobutyric acid (GABA) and glutamate also play crucial roles. GABA is the brain’s natural “calming” neurotransmitter, helping to reduce neural activity and induce relaxation. Substances like alcohol and benzodiazepines (medications often prescribed for anxiety) enhance the effects of GABA, making a person feel relaxed or sedated. Over time, the brain becomes less capable of producing GABA naturally, leading to increased anxiety and stress when the substance is not present.
On the other hand, glutamate is involved in learning and memory, and many addictive substances affect glutamate signalling, further altering how the brain functions long-term. The imbalance of these neurotransmitters due to substance abuse causes cognitive impairments, mood swings, and memory issues, making it even harder for someone to break the cycle of addiction.
Why Some People Are More Prone to Addiction
Addiction arises from a complex interaction between genetics, environmental factors, and brain chemistry. While anyone can develop an addiction, some people are more prone to genetic factors. Studies suggest that individuals with a family history of addiction are more likely to become addicted themselves because they may have inherited a brain structure or function that predisposes them to addictive behaviours.
Additionally, mental health conditions like anxiety or depression often go hand in hand with addiction. Someone dealing with chronic stress or depression might use substances to cope, unknowingly setting themselves up for addiction by altering their brain’s chemistry over time.
Case Study: Opioid Addiction Epidemic
The opioid epidemic in many parts of the world, including the U.S. and India, is a stark example of how addiction can take hold. Opioids, which include prescription painkillers like morphine and illegal drugs like heroin, bind to specific receptors in the brain, blocking pain signals and creating feelings of euphoria. The widespread availability of these drugs, especially through overprescription, has led to a surge in addiction cases.
As the brain becomes dependent on opioids to release dopamine and regulate mood, individuals find it almost impossible to quit without help. In severe cases, overdose can occur, leading to respiratory failure and death. This epidemic highlights the urgent need for better understanding and treatment of addiction.
The Road to Recovery: Rewiring the Brain
The good news is that the brain is capable of healing itself to some extent. With the right treatment—counselling, medication, and lifestyle changes—it’s possible to restore a balance in brain chemistry. Medications such as methadone and buprenorphine are effective in treating opioid addiction by regulating dopamine levels without causing the harmful side effects associated with the addictive substance.
Moreover, Cognitive Behavioral Therapy (CBT) and mindfulness practices help individuals manage cravings and triggers, while long-term strategies like exercise, proper nutrition, and strong social support help rebuild the brain’s natural reward system.
Conclusion
Addiction is not a moral failing but rather a chemical process that takes over the brain’s reward system. The good news is that with understanding, compassion, and the right tools, recovery is possible. The chemistry of addiction explains how substances hijack our brains, but it also shows that healing can happen. If you or someone you know is struggling with addiction, don’t hesitate to seek help. Addiction is a medical condition that deserves attention, not judgment.
Author’s Note
Writing about addiction has been an eye-opener for me, reminding us that our brains are complex and beautiful yet vulnerable. If this blog has made you think about addiction differently, then I’ve done my job. Let’s continue to support each other in understanding the science behind behaviours that impact lives.
G.C., Ecosociosphere contributor.
References and Further Reading
- Mayo Clinic: Substance Use Disorders
- There’s a Reason For Your Urge To Keep Scrolling Through Your Smartphone’s News Feed – BLOGEMONIUM. https://www.blogemonium.com/2023/08/theres-reason-for-your-urge-to-keep.html
- Drug Overdose Statistics and How You Can Help | PA Recovery. https://pennsylvaniarecoverycenter.org/drug-overdose-statistics-and-how-you-can-help/
- Behind the Wheel: The Impact of Prescription Drugs on Driving | UseMyPro.com. https://usemypro.com/behind-the-wheel-the-impact-of-prescription-drugs-on-driving.htm