Fun Fact: Did you know that scientists have successfully used stem cells to help a patient with type 1 diabetes produce her own insulin for the first time?
It sounds like something from a science fiction novel, but it’s reality. In a groundbreaking medical breakthrough, researchers have developed a stem cell therapy that may change the future of diabetes treatment. A recent study published in the journal Cell describes how a 25-year-old woman with type 1 diabetes—a condition where the body’s immune system destroys insulin-producing cells—was able to produce her own insulin for the first time in years after receiving a stem cell transplant.
This is the first successful treatment of type 1 diabetes using stem cells, and it offers hope for millions of people worldwide who rely on insulin injections to manage their condition. But how did this therapy work, and what does it mean for the future of diabetes treatment? Let’s explore this exciting new development.
Understanding Type 1 Diabetes
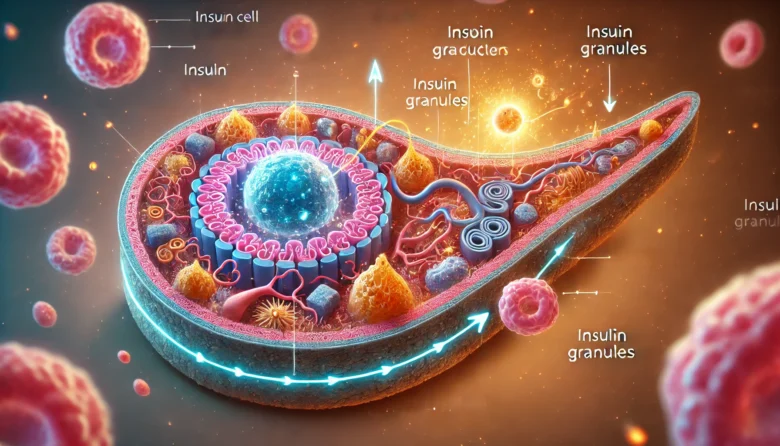
Before diving into the breakthrough, it’s important to understand the challenge posed by type 1 diabetes. This autoimmune condition arises when the body’s immune system mistakenly targets and destroys beta cells within the pancreas. These beta cells play a crucial role in producing insulin, the hormone that helps regulate blood sugar. In the absence of insulin, blood sugar levels can rise to dangerous levels, resulting in complications like heart disease, nerve damage, and kidney issues.
For years, people with type 1 diabetes have relied on regular insulin injections or insulin pumps to manage their condition. However, these treatments do not restore the body’s ability to produce insulin naturally, making the search for a more permanent solution a priority for researchers.
The Breakthrough: Stem Cells as a Solution
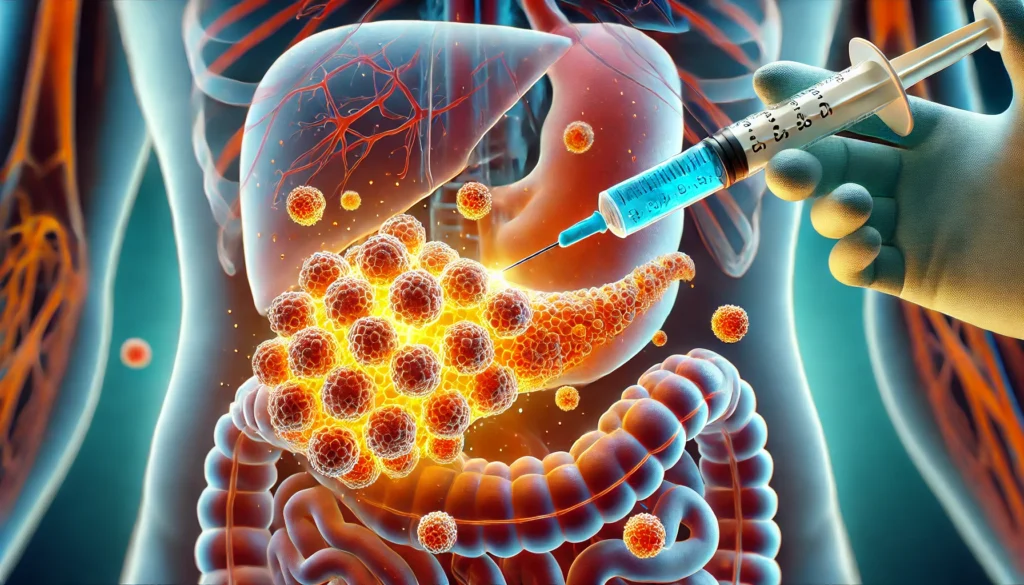
This recent study offers a glimmer of hope for a future where type 1 diabetes could potentially be reversed. Led by scientists based in China, the study involved a process that used induced pluripotent stem cells (iPS cells) to create insulin-producing cells.
Induced pluripotent stem cells are essentially “blank” cells that can be re-engineered to develop into any cell type within the body. The researchers extracted cells from three individuals with type 1 diabetes and reprogrammed them into iPS cells. From there, they generated 3D clusters of islets—the group of cells in the pancreas that contain beta cells capable of producing insulin.
Once the islet clusters were developed, they were transplanted into the abdomen of the 25-year-old woman. In a stunning result, the woman began producing her own insulin within just two and a half months of the procedure. Even more impressively, she has been able to maintain her insulin production for over a year without needing additional insulin injections.
A Case Study in Success
This case marks a historic first in the treatment of type 1 diabetes with stem cells. The woman, who had been living with the disease for years, no longer required insulin injections to control her blood sugar. According to the study, her body is now producing sufficient insulin to regulate her glucose levels naturally. This outcome is remarkable, as it shows that reprogrammed stem cells can successfully replace damaged beta cells and restore insulin production.
It’s worth noting that while this is an extraordinary step forward, researchers are cautiously optimistic. As Jay Skyler, an endocrinologist at the University of Miami, points out, the results will need to be replicated in larger studies before this therapy can be widely adopted. Skyler also emphasized the need to monitor the patient for several more years to ensure that her insulin production continues. If the treatment proves to be durable over time, it could signal a major shift in how we treat type 1 diabetes.
The Science Behind Stem Cell Therapy
So, how exactly did these researchers use stem cells to reverse diabetes? The process started with the extraction of cells from the patients, which were then reprogrammed into pluripotent stem cells. This reprogramming process essentially “resets” the cells, allowing them to transform into other types of cells, including the insulin-producing beta cells needed by patients with diabetes.
Once the pluripotent stem cells were generated, they were chemically guided to become clusters of islet cells, which contain the beta cells that produce insulin. These islet clusters were then transplanted into the patient’s abdomen. Once inside the body, the newly created beta cells began producing insulin, restoring the body’s ability to regulate blood sugar naturally.
This approach could be life-changing for millions of people who live with type 1 diabetes. Unlike current treatments, which require ongoing insulin injections, stem cell therapy offers the potential to restore natural insulin production for years—perhaps even permanently.

Challenges and Future Prospects
While the results of this study are promising, there are still challenges to be addressed. For instance, one concern is whether the patient’s immune system will eventually reject the transplanted cells, as type 1 diabetes is an autoimmune condition. To prevent this, patients receiving stem cell transplants may need to take immunosuppressant drugs to protect the new beta cells from being attacked.
Moreover, stem cell therapy is currently expensive, and it may take some time before it becomes a widely affordable and accessible treatment option. Nonetheless, the potential benefits are immense, and further research could refine the process, making it more affordable and available to a broader population.
Conclusion: A New Era for Diabetes Treatment?
The success of this stem cell therapy offers hope for the millions of people affected by type 1 diabetes. If further studies confirm the long-term effectiveness of this treatment, it could revolutionize the way we manage this condition, moving away from daily insulin injections and toward a more permanent solution.
While we’re still in the early stages of research, the possibilities are exciting. This breakthrough represents not just a step forward for diabetes treatment but a leap toward a future where regenerative medicine can reverse or even cure chronic diseases.
Author’s Note
As someone who has followed advancements in medical research for years, I believe this breakthrough in stem cell therapy for diabetes is nothing short of revolutionary. I hope this article gives you a sense of the incredible potential that science holds for changing lives.
G.C., Ecosociosphere contributor.
References and Further Reading
- Stem Cell Research for Diabetes
- American Diabetes Association
- Yang, L., Hu, Z. M., Jiang, F. X., & Wang, W. (2022). Stem cell therapy for insulin-dependent diabetes: Are we still on the road? https://core.ac.uk/download/534155349.pdf
- Type 1 Diabetes Cure: Current Research (2024). https://www.dvcstem.com/post/type-1-diabetes-cure
- Stem Cell Therapy for Type 1 Diabetes | Stem Cell Therapy for Type 1 Diabetes. https://avani-cryoviva.gitbook.io/stem-cell-therapy-for-type-1-diabetes
- Can stem cells ‘cure’ diabetes? Lessons from two trials