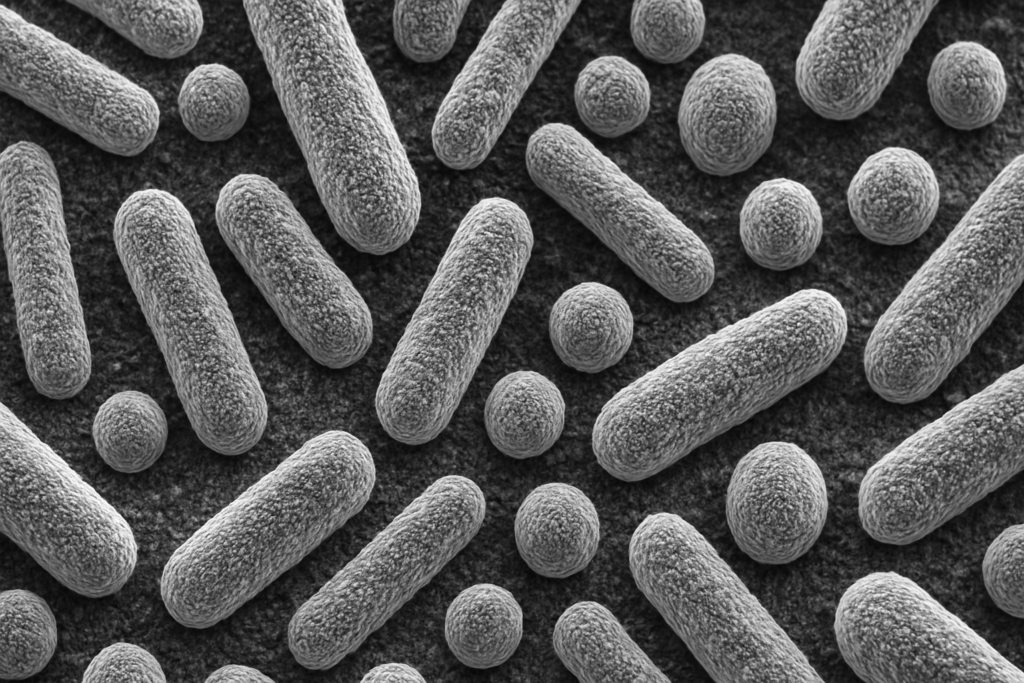
Fun Fact: The human gut hosts around 100 trillion bacteria, outnumbering human cells by more than 10 to 1!
Imagine spending years trapped in your own body by relentless, unexplained pain. No visible injury, no clear diagnosis—just daily agony that painkillers barely touch. Now imagine that the solution might not be found in a powerful new drug or complex surgery, but in something shockingly simple: healthy gut bacteria.
Sounds crazy? Maybe. But welcome to the new frontier of chronic pain treatment, where hope is brewing not in pharmaceutical factories, but deep inside the human gut. Recent research suggests that rebalancing our internal ecosystems could ease conditions like fibromyalgia, a notoriously mysterious and debilitating disorder. And it’s a breakthrough that’s making doctors and patients alike rethink everything they know about pain.
Fibromyalgia: The Pain That Medicine Forgot
For decades, fibromyalgia has baffled doctors and frustrated patients. It affects up to 4% of the global population, and causes:
- Widespread muscle pain
- Fatigue
- Sleep disturbances
- Brain fog and depression
Yet, standard medical tests usually show nothing wrong. No swelling. No broken bones. No obvious injury. As a result, patients are often dismissed, misdiagnosed, or worse—told it’s “all in their heads.”
One such patient is Rina Green, a 38-year-old woman from Haifa, Israel. What started as a mild backache spiralled into full-body agony that left her wheelchair-bound. Conventional treatments—painkillers, physical therapy—offered little relief. Her life, she says, became a “living hell.”
Until she swallowed a capsule filled with gut bacteria.
A Radical New Approach: Healing from the Inside Out
Earlier this year, Green took part in a small experimental trial led by scientists at the Technion — Israel Institute of Technology. The treatment?
Pills containing living microorganisms extracted from the healthy guts of other women.
After a few months of regular dosing, something astonishing happened:
- Her pain dramatically decreased.
- She could walk again—something she hadn’t done since her diagnosis.
- Sleep improved. Anxiety lessened.
Green wasn’t alone. Out of 14 women in the trial, 12 reported significant symptom improvement.
If it sounds too good to be true, you’re not alone in thinking it. Scientists themselves are cautious, but they are also quietly thrilled. As Amir Minerbi, a pain researcher and co-lead of the study, says:
“It’s preliminary, but it’s encouraging enough to move forward.”
So, How Can Gut Bacteria Affect Pain?
It seems absurd, right? How can bugs in your intestines change how your back or legs feel?
Here’s the science:
- Your gut is home to a microbiome—a vast community of bacteria, viruses, and fungi.
- These microbes produce chemicals that regulate everything from digestion to brain function.
- Some bacteria influence immune system signals that control inflammation and nerve sensitivity.
When gut bacteria go wrong—due to diet, stress, antibiotics, or genetics—they may tip the body’s systems into overdrive, heightening pain perception even when no physical injury exists.
In fact, earlier experiments showed that mice injected with gut microbes from patients with fibromyalgia developed greater sensitivity to pain compared to mice injected with gut microbes from healthy individuals.
The Clinical Trial: What Really Happened
Let’s break it down:
Step One:
Participants received antibiotics to wipe out large portions of their existing gut bacteria.
Step Two:
Over the next ten weeks, they swallowed capsules filled with microbes from healthy human donors.
Step Three:
Researchers monitored their symptoms—pain levels, anxiety, sleep quality, and fatigue.
The results?
- 12 of 14 reported reduced pain.
- Many also saw improvements in anxiety and sleep.
- Some reported mild fatigue as a side effect.
Is it a miracle? No. There was no control group (no placebo), and participants knew they were receiving the treatment, which may have biased the results.
Still, for people whose pain had resisted every other therapy, the improvements were remarkable.
What Experts Are Saying
Andreas Goebel (pain scientist at University of Liverpool):
“Usually, treatment-resistant fibromyalgia patients don’t respond to anything. This is going in the right direction.”
Katelyn Sadler (neuroscientist at University of Texas at Dallas):
“It definitely demonstrates that the microbiome is at least one of many factors contributing to pain. That’s a big, exciting finding.”
Translation:
While not a magic bullet, this is real science pointing to a new avenue of treatment.
Why It Matters So Much
Think about it:
- Fibromyalgia patients are often gaslit. Their pain is dismissed as imaginary.
- Painkillers only mask symptoms. They don’t cure the underlying problem, and come with serious side effects.
- Gut microbiome therapy could be safer. No opioids. No steroids. Just restoring biological balance.
This research offers not just hope but validation for millions suffering from invisible illnesses.
It also invites a radical rethinking:
Is pain purely neurological, or is it microbial too?
Challenges Ahead
Before you rush out to buy probiotics, slow down.
- Small sample size: Only 14 people. Larger studies are needed.
- No placebo group: Results could be partly psychological.
- Long-term effects unknown: Will the benefits last? Are there risks we don’t know yet?
That’s why Minerbi and his team are launching a larger trial with 80 participants, including proper controls.
The goal? Identify specific bacterial strains that cause or relieve pain, leading to precision gut therapies in the future.
Conclusion: A Gut Feeling That Could Change Everything
This is more than just a scientific curiosity. It’s a lifeline for those trapped in pain.
It’s a revolution in medicine’s understanding of the gut-brain connection.
And it’s a reminder: Sometimes, the most powerful therapies are already inside us—waiting to be understood.
So the next time you hear someone say, “It’s all in your head,” you might just smile and reply,
“Actually, it might be all in my gut.”
Author’s Note:
As someone who has seen close friends struggle with invisible illnesses like fibromyalgia, this research fills me with cautious hope. Science still has a long way to go, but if healing really starts in the gut, maybe we’re finally on the right path.
G.C., Ecosociosphere contributor.