Fun Fact: Every brain has nearly 100 billion neurons, but just losing a few thousand in the right area can lead to Parkinson’s disease.
Imagine if doctors could transplant new, healthy brain cells into people with Parkinson’s disease without the body fighting back. Now imagine those cells also came with a built-in kill switch—just in case something went wrong. Sounds like science fiction? A newly published study in Cell Stem Cell suggests that this breakthrough could become a reality sooner than expected.
Researchers have successfully engineered human neurons that are invisible to the immune system and transplanted them into rats with Parkinson’s-like symptoms. Even more impressive, these cells not only survived, they actually restored lost muscle control. Let’s break down this major milestone and understand why it could change the way we treat degenerative brain diseases like Parkinson’s.
Understanding Parkinson’s Disease
Parkinson’s disease is a progressive disorder that primarily affects movement. It occurs when specific neurons in the brain, responsible for producing dopamine (a chemical messenger), begin to die. Without enough dopamine, the brain struggles to control muscles, leading to symptoms such as tremors, stiffness, and difficulty walking.
While existing options such as medication and deep brain stimulation help control symptoms, they neither cure the condition nor halt its advancement. That’s why scientists are exploring cell-replacement therapies—introducing new dopamine-producing neurons to replace the ones that have died.
But here’s the catch: introducing foreign cells into the body usually triggers the immune system to attack them, just as it would with bacteria or viruses. To prevent this, patients must take immunosuppressant drugs for life, which come with risks like infections and even cancer.
The Promise of a Universal Cell Therapy
What if we could transplant cells into any patient, without worrying about rejection? That’s the idea behind a universal cell line—a type of engineered cell that’s compatible with everyone. And that’s exactly what the team led by Dr. Clare Parish at the Florey Institute of Neuroscience and Mental Health in Melbourne, Australia, is working toward.
The Florey Institute is one of Australia’s leading research centers dedicated to brain and mental health.
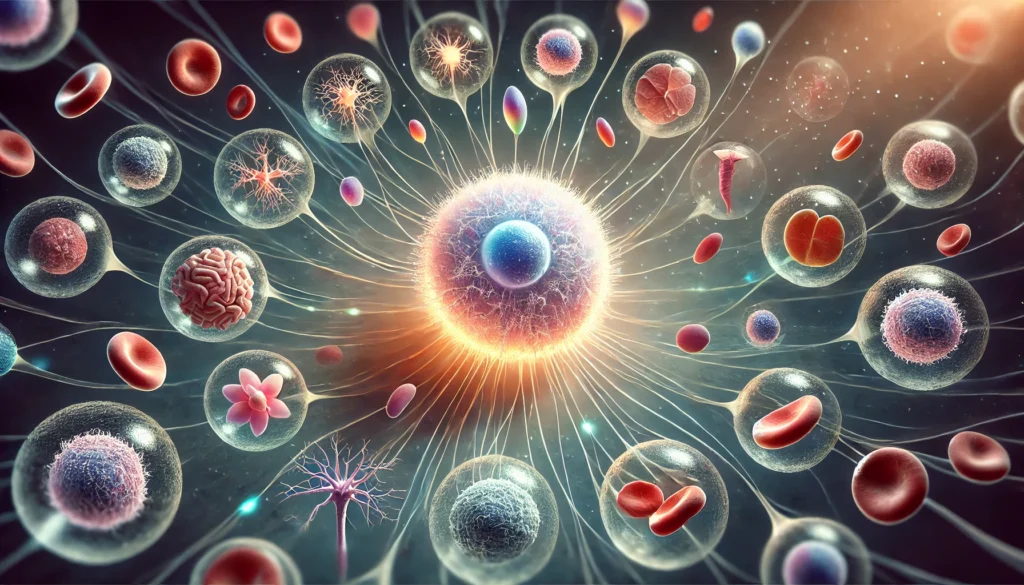
In their latest research, the team focused on modifying human pluripotent stem cells—which have the potential to become nearly any type of cell—into dopamine-producing neurons specifically suited for Parkinson’s therapy. But instead of leaving the cells vulnerable to immune attack, the team gave them something extraordinary—a genetic invisibility cloak.
How the Invisibility Cloak Works
The researchers altered eight specific genes in these stem cells. These genes are known to help the placenta and cancer cells avoid being detected and destroyed by the immune system.
By enhancing the activity of these genes, the engineered brain cells essentially became invisible to immune cells, like stealth jets flying under the radar. The result? The rats’ immune systems did not reject the implanted neurons, even when their immune systems were partially replaced with human immune cells to better mimic real human reactions.
This kind of gene editing is groundbreaking. It means that, in the future, we could have off-the-shelf cell therapies ready to treat people without having to customize them for each individual or suppress their immune systems.
Testing the Therapy in Parkinson’s Rats
To simulate Parkinson’s disease, researchers used a neurotoxin that damages dopamine neurons in rats, causing movement problems. After injecting the engineered neurons into the rats’ brains, they waited 12 weeks.
The results were remarkable.
The rats showed significant improvement in motor function. That means the new cells were not only surviving but were also functioning correctly, producing dopamine and integrating into the brain’s communication network.
This is a big leap forward. It shows that these cloaked neurons can do what they’re supposed to do inside a living brain.
Safety First: The Suicide Gene
Now, any time we start tinkering with genes—especially altering eight of them—safety becomes a top priority.
One major concern is that these invisible cells might become too invisible. If they go rogue or turn cancerous, the body wouldn’t be able to detect and destroy them.
To solve this, the team added a ninth gene—a “suicide gene”. This gene acts as a safety switch. If needed, doctors can give the patient a common antiviral drug called ganciclovir, which activates the suicide gene and causes the cells to stop dividing.
In tests, this safety mechanism worked exactly as intended. When the rats were given ganciclovir, the transplanted cells stopped growing.
This gives researchers, doctors, and regulatory agencies peace of mind that the therapy can be controlled even after transplantation.
The Bigger Picture: Why This Matters
This research goes far beyond Parkinson’s disease. If we can make universal donor cells that are immune-evasive and come with built-in safety features, we can potentially treat:
- Type 1 and Type 2 diabetes, by transplanting insulin-producing pancreatic cells.
- Heart failure, by replacing damaged heart muscle cells.
- Macular degeneration, by introducing retinal cells to restore vision.
These universal cells could also simplify logistics. Instead of creating custom stem cells for each patient—a time-consuming and expensive process—we could have ready-to-go cell lines, much like universal blood types.
Challenges Ahead
As promising as this is, it’s not ready for hospitals just yet.
One major hurdle is regulatory approval. As Dr. Clare Parish rightly pointed out, getting approval for a product that involves altering nine genes is no small task. Regulatory bodies need to be convinced that such therapies are both safe and effective.
Moreover, while results in rats are exciting, we need to see how these cells behave in larger animals and, eventually, in human clinical trials. The long-term impact, stability of the transplanted cells, and potential side effects must all be studied.
But make no mistake—this is a huge step forward.
Conclusion: Toward a Future Without Rejection
The idea of an “invisibility cloak” for brain cells sounds like something out of a superhero comic, but it’s becoming a reality. This new research brings us one step closer to a world where cell therapy is not only effective but also safe, universal, and accessible.
Parkinson’s disease affects millions of people worldwide. Current treatments help manage symptoms but don’t solve the underlying problem. With advances like these, we may soon have the tools to repair the brain, not just treat its symptoms.
The future of regenerative medicine is bright, and this study gives us a glimpse into what that future might look like.
Author’s Note
With ongoing discoveries about the brain and immune system, we are stepping into a transformative era where complex conditions like Parkinson’s may be addressed at the cellular level. This blog aims to explain cutting-edge research in simple language so that more people can appreciate and understand the exciting developments happening in health and biotechnology.
G.C., Ecosociosphere contributor.
References and Further Reading
- Nature News Article:
https://doi.org/10.1038/d41586-025-01080-5 - Original Research in Cell Stem Cell Journal (link from the article):
https://www.cell.com/cell-stem-cell - Understanding Parkinson’s Disease: A Guide for Caregivers. https://www.idealcaregivers4u.com/post/understanding-parkinson-s-disease-a-guide-for-caregivers