Fun fact: Did you know that skipping breakfast—a habit many of us already have—can be rebranded as a “diet plan” called intermittent fasting?
Intermittent fasting, especially the 16:8 method (16 hours of fasting and 8 hours of eating), has been hailed as everything from a weight-loss secret to a brain-boosting miracle. But recent studies have also thrown up a worrying headline: fasting this way might actually increase your risk of heart disease. So, which is it? A magic bullet or a silent hazard?
The Promise of 16:8 Fasting
The popularity of intermittent fasting exploded in the last decade. Social media fitness influencers flaunt toned bodies and credit their discipline to eating only between, say, 12 pm and 8 pm. Science, too, has given it some early applause.
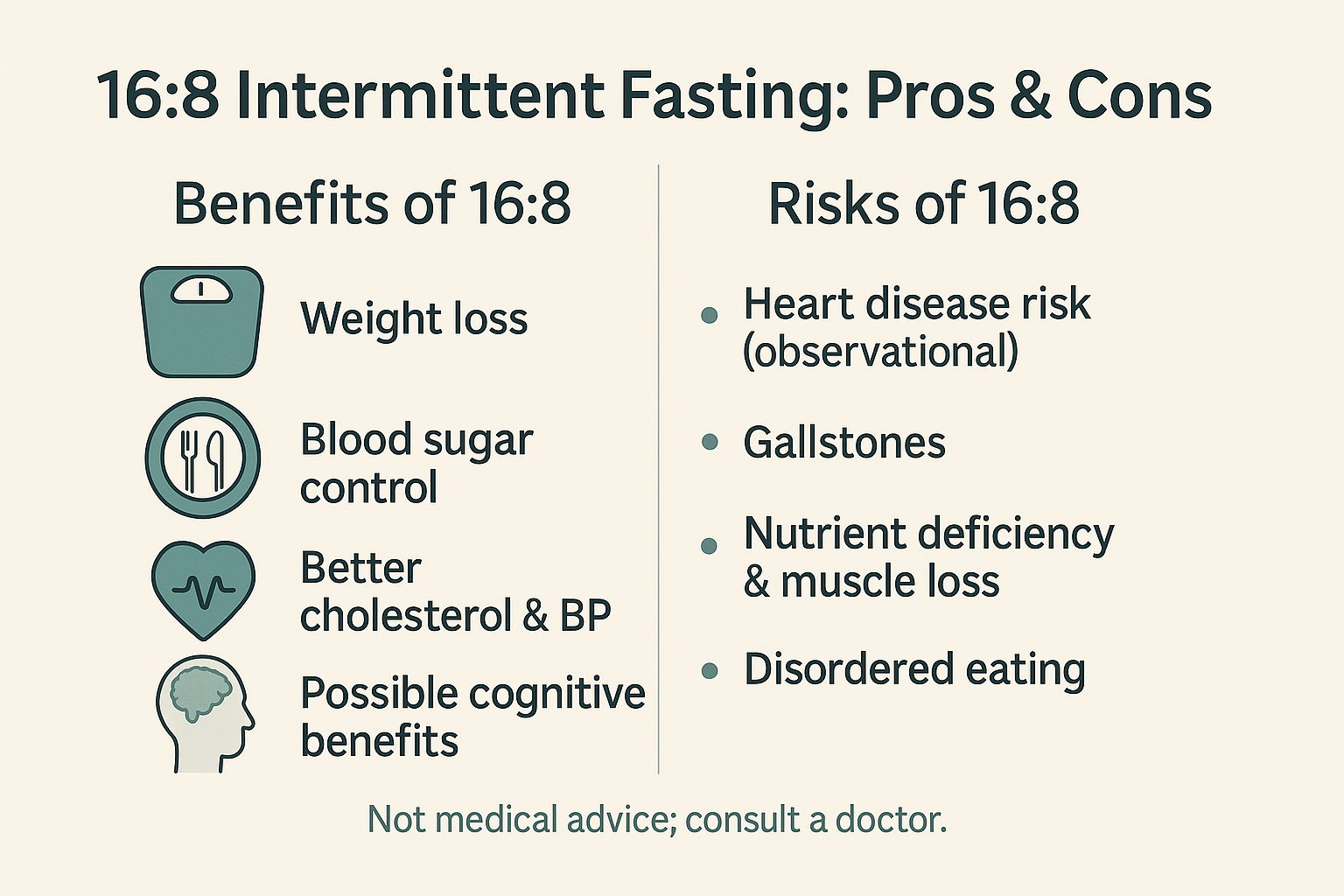
Weight loss without calorie counting: By compressing eating into an 8-hour window, people naturally eat less, leading to modest but noticeable fat loss. A study in 2023 found intermittent fasting helped reduce waist circumference and body fat while improving cholesterol and insulin sensitivity.
Sharper minds and healthier brains: Animal studies show fasting reduces harmful proteins linked to Alzheimer’s disease. Human studies are smaller but suggest better memory and focus after a few weeks of fasting. Imagine a diet that promises not just a slimmer waistline but a sharper brain. Tempting, isn’t it?
Blood sugar and diabetes control: Intermittent fasting seems to lower fasting insulin levels and improve how the body handles sugar. That’s crucial for people at risk of type 2 diabetes.
So far, so good. The narrative sounds almost utopian: eat less often, live longer, think clearly. But then comes the twist.
The Darker Side of Fasting
Science rarely leaves us with fairy tales, and intermittent fasting is no exception.
A large U.S.-based study (20,000 adults) dropped a bombshell: people who ate all their meals in less than 8 hours a day had a 91% higher risk of dying from cardiovascular disease compared to those who ate over 12–16 hours. That’s right—your shortcut to a slimmer waist might come with a bigger bill: your heart.
It’s not just the heart. Doctors also warn about:
Gallstones and gallbladder issues—prolonged fasting can cause bile to sit idle, forming stones.
Nutrient deficiencies—if you cram your meals into 8 hours and don’t eat smart, you might skip key vitamins and proteins.
Muscle loss—one trial showed faster loss of lean muscle than fat if protein intake wasn’t adequate.
Disordered eating patterns—fasting may trigger binge eating during the eating window, fuelling guilt and yo-yo dieting.
Suddenly, the miracle diet doesn’t feel so miraculous anymore.
Short-Term Gains, Long-Term Unknowns
It’s easy to see why people love 16:8 fasting: the initial rewards are real. You feel lighter, maybe sharper, and your blood pressure or cholesterol numbers might dip. But the long-term picture is murky.
Authorities like the Mayo Clinic (a U.S.-based nonprofit medical research center) and the National Institute on Aging (a U.S. government research body) both caution that there isn’t enough evidence to recommend fasting for longevity. Sure, it works for some people, but science doesn’t yet know what happens after ten or twenty years of daily 16-hour fasts.
And that’s the unsettling truth: we are in the middle of a giant, unsupervised experiment.
So, Should You Fast?
Here’s the honest answer: it depends.
If you’re young, overweight, and otherwise healthy, a 16:8 fast might help you shed kilos and reboot your metabolism—if you eat nutritious meals and don’t binge.
If you already have heart disease, diabetes, or gallbladder issues, tread carefully. The risks may outweigh the rewards.
If you’re an older adult or prone to disordered eating, fasting might do more harm than good.
What we can say for sure is this: fasting is not a magic bullet. A balanced diet, regular exercise, and good sleep are still the timeless formula for health.
Conclusion: Beyond the Hype
Intermittent fasting 16:8 has become the darling of the diet world, with promises of quick weight loss and even brain protection. But as the latest evidence suggests, it may not be the universal health hack it’s advertised to be.
The truth lies somewhere in the messy middle: fasting can help some, harm others, and confuse most of us. Maybe the real question isn’t “Should I fast?” but “Why am I fasting?” Is it to feel better, look better, or because an influencer said so?
Diet trends come and go, but your heart, your brain, and your body will be with you for life. Treat them with care, not experiments.
Author’s Note
As someone who has watched diet fads rise and fall, I find the story of 16:8 fasting fascinating. It exposes our deep desire for simple solutions to complex health problems. But health, like life, rarely fits into an 8-hour window.
G.C., Ecosociosphere contributor.
References and Further Reading
- Mayo Clinic – Intermittent fasting: What are the benefits?
- National Institute on Aging – Research on fasting and longevity
- American Heart Association News – Study on time-restricted eating and heart risk
- Intermittent fasting as effective for weight loss as traditional dieting
- High Cholesterol and High Blood Pressure – WebMD
- Is Intermittent Fasting Evidence-Based?
- Diet, Sleep and Exercise: The Keystones of Healthy Lifestyle