Have you ever wondered why some people can eat peanuts without any issues while others have a life-threatening allergic reaction? Or why do certain individuals develop chronic diseases where their immune system attacks their own body? These conditions fall under the fascinating yet complex realm of allergies and autoimmune diseases.
In this blog, we’ll explore the science behind these conditions, uncovering why they occur, how they differ, and what’s being done to manage them. Understanding the science behind allergies and autoimmune diseases helps shed light on how our immune system, designed to protect us, sometimes turns against us.
The Immune System: A Double-Edged Sword
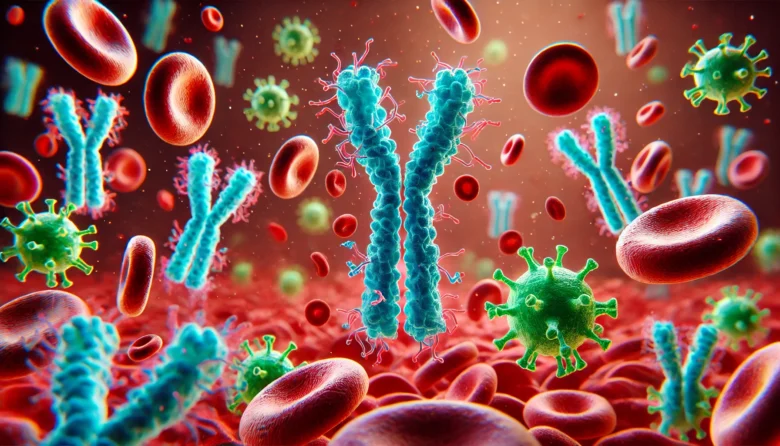
The immune system is like a personal bodyguard, constantly on alert for harmful invaders like bacteria, viruses, and other pathogens. It identifies threats and neutralizes them, keeping us healthy. But sometimes, this finely tuned system misfires, leading to conditions such as allergies and autoimmune diseases.
What Happens During an Allergic Reaction?
Allergies occur when the immune system mistakenly treats harmless substances—such as pollen, pet dander, or certain foods—as dangerous invaders. This substance is called an allergen. The immune system overreacts by producing an antibody called immunoglobulin E (IgE), which binds to the allergen and triggers a series of reactions in the body, including the release of histamines. Histamines cause classic allergic symptoms like sneezing, itching, and swelling.
Think of it as a false alarm: the immune system is acting like there’s an intruder, but it’s really just reacting to something harmless.
Case Study: Peanut Allergies
One of the most well-known allergic reactions is the peanut allergy, which can be severe and even life-threatening. In this case, the body identifies peanut proteins as harmful, and the immune response can lead to anaphylaxis, a serious condition where the airways can close up, making breathing difficult. This is why people with peanut allergies carry epinephrine auto-injectors (commonly known as EpiPens), which help counteract the body’s extreme reaction by relaxing the muscles and reducing swelling.
Autoimmune Diseases: When the Body Turns on Itself
In autoimmune diseases, the immune system’s confusion runs much deeper. Rather than targeting an external allergen, the immune system begins attacking the body’s own cells, tissues, and organs as though they were harmful intruders. This is not a one-time reaction but an ongoing battle.
Common Autoimmune Conditions
Rheumatoid Arthritis (RA): In this condition, the immune system targets the joints, leading to inflammation, pain, and eventual joint damage. RA affects millions of people worldwide, and it’s an example of how the immune system mistakenly targets healthy tissue.
Type 1 Diabetes (T1D): In Type 1 diabetes, the immune system destroys the insulin-producing cells in the pancreas. Without insulin, the body can’t properly regulate blood sugar, leading to a range of serious health issues. Type 1 diabetes often develops in children and young adults, and while there is no cure, treatments focus on insulin therapy and blood sugar management.
Lupus (Systemic Lupus Erythematosus or SLE): Lupus is a condition where the immune system can attack virtually any part of the body, including the skin, joints, and internal organs. The symptoms are widespread and can range from rashes to organ failure, making lupus a particularly challenging condition to manage.
These autoimmune conditions illustrate how the immune system, which is usually protective, can become dysfunctional.
What Causes Allergies and Autoimmune Diseases?
The exact causes of both allergies and autoimmune diseases are still a subject of intense research, but scientists believe they result from a combination of genetic and environmental factors.
The Role of Genetics
Both allergies and autoimmune diseases often run in families, suggesting a strong genetic component. If your parents have allergies, for example, you’re more likely to develop them too. Similarly, autoimmune diseases like rheumatoid arthritis and lupus tend to occur more frequently in certain genetic groups.
Environmental Triggers
Environmental factors also play a significant role. For allergies, things like pollution, diet, and early exposure to allergens are believed to influence how the immune system develops. In the case of autoimmune diseases, infections or exposure to certain chemicals might trigger an abnormal immune response in someone who is genetically predisposed.
The Hygiene Hypothesis
One popular theory to explain the rise in both allergies and autoimmune diseases is the hygiene hypothesis. This theory suggests that growing up in an overly sanitized environment—without enough exposure to bacteria and pathogens—may hinder the development of a robust immune system. In other words, our immune systems are not “trained” properly, which may cause them to overreact to harmless substances or attack the body’s own cells.
Managing Allergies and Autoimmune Diseases
Treatment Options for Allergies
Managing allergies usually involves two approaches: avoiding the allergen and treating the symptoms. Antihistamines (medications that block the effects of histamines) are commonly used to treat allergic reactions. In severe cases, like peanut allergies, immunotherapy may be recommended. This involves exposing the immune system to small amounts of the allergen over time to train it to stop overreacting.
Anecdote: A friend of mine used to suffer terribly from seasonal allergies every spring. It got to the point where he couldn’t go outside without sneezing and itching non-stop. Eventually, he tried allergy shots (a form of immunotherapy) and saw a huge improvement. Now, springtime isn’t such a nightmare for him anymore!
Treatment for Autoimmune Diseases
For autoimmune diseases, treatment is more complex. Since the immune system is attacking the body, most therapies aim to suppress the immune response. Medications like corticosteroids and immunosuppressants are commonly used to reduce inflammation and prevent further damage.
For example, in rheumatoid arthritis, biologic drugs like etanercept (sold by Amgen) and adalimumab (sold by AbbVie under the brand name Humira) target specific parts of the immune system to reduce inflammation and prevent joint damage.
Diet, exercise, and lifestyle modifications can also play a role in managing autoimmune conditions, helping reduce flare-ups and improve quality of life.
Conclusion: A Delicate Balance
The science behind allergies and autoimmune diseases reveals how complex our immune system truly is. While it is designed to protect us, sometimes it gets confused, leading to conditions that can be mild or life-threatening. Ongoing research continues to uncover the causes and treatments for these conditions, offering hope for better management and even prevention in the future.
If you or someone you care about is affected by allergies or an autoimmune disease, it’s important to stay up to date on the latest treatment options and research. Our understanding of the immune system is evolving, and with it, our ability to manage these challenging conditions.
Author’s Note
Learning about how the immune system works is both fascinating and eye-opening. I hope this blog has helped you better understand allergies and autoimmune diseases, whether you or a loved one are affected by them. Scientific advancements are being made in these areas, and staying informed plays a vital role in managing your health.
G.C., Ecosociosphere contributor.
References and Further Reading
- What Causes Autoimmune Disease? – National Institutes of Health (NIH)
- What is Antibody or Immunoglobulin Therapy?. https://www.berkeleyformula.com/immune-health/what-is-antibody-or-immunoglobulin-therapy/